Healthcare systems are on the frontline during crises—from flood-related cholera outbreaks to earthquake injuries and zoonotic diseases. When essential services falter, lives are at risk: in 2020 alone, pandemic disruptions meant 1.4 million fewer people received tuberculosis care across 80 countries. These shocks highlight the urgent need for resilient health systems with functioning facilities, staff, supplies, data, and reliable power and water, supported by strong governance and clear policies.
Resilient healthcare also depends on lifeline infrastructure. The Climate and Disaster Risk Management for Health Systems thematic area strengthens this resilience by generating analytics, tools, and evidence that identify gaps, prioritize actions, and inform investments. Our mission is to build resilient health systems and critical infrastructure through integrated analytics, advisory services, and operational support. We work with governments, development partners, and communities to diagnose vulnerabilities, design practical solutions, and support investments that ensure equitable healthcare access before, during, and after crises. Our three main objectives are to:
- Strengthen healthcare resilience to ensure uninterrupted essential services during crises and reduce illness, deaths, and socioeconomic impacts.
- Advance evidence-based solutions by developing and applying analytics, diagnostics, and tools to identify vulnerabilities and guide resilient investments.
- Build integrated partnerships with governments, industry partners, and communities to implement cross-sectoral solutions for equitable healthcare access during shocks.
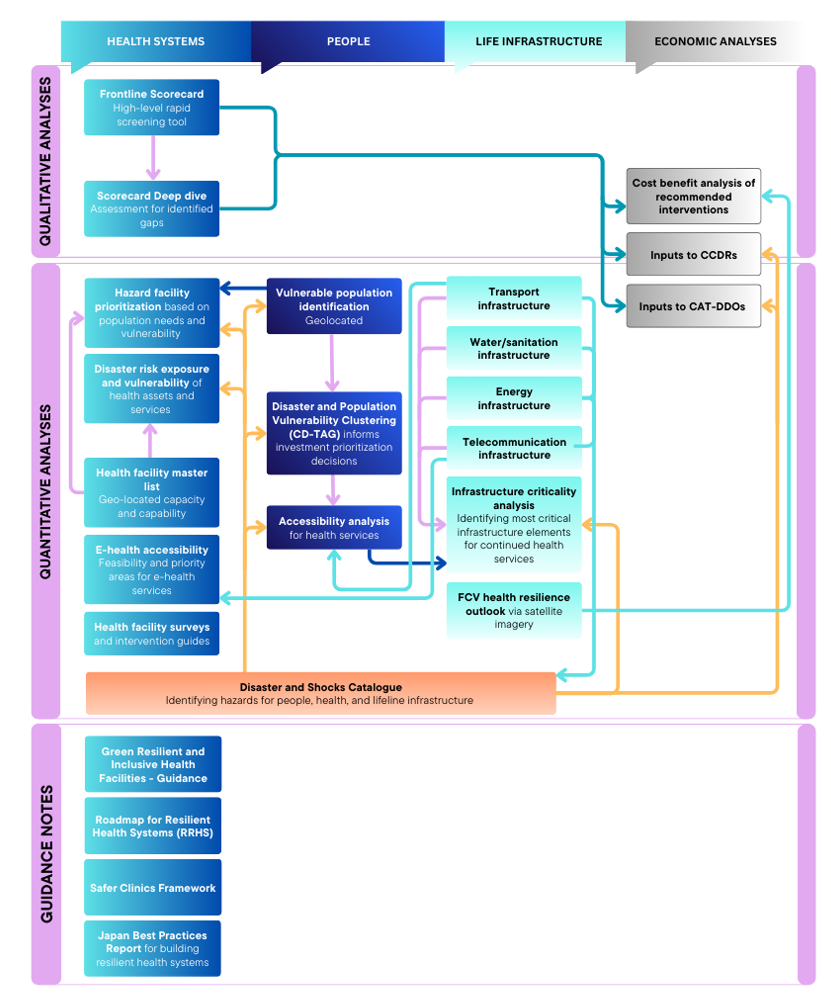
The Climate and Disaster Risk Management for Health Systems thematic area operationalizes the World Bank Group’s crisis resilience agenda for the health sector. Using service delivery, geospatial modeling, health infrastructure exposure and (e)-accessibility, population vulnerability analysis, and sector-specific simulations, the thematic area translates climate and disaster risks into prioritized, resilient health investments. By linking health systems with lifeline infrastructure and integrating built environments and regulatory and planning measures, the thematic area enables task team leads within the World Bank Group to scope, design and implement operations that protect essential services, unlock contingent financing, and strengthen system resilience before, during, and after shocks. The thematic area also provides decision-ready analytics and corporate products and indicators to health teams supporting operational needs at the World Bank Group.
Highlights

Watch the Climate and Disaster Risk Management for Health Systems videos playlist on YouTube
Services and Tools
1. Rapid Assessment
The Frontline Scorecard is the World Bank Group’s country baseline rapid assessment tool that gauges a country’s health system resilience to natural hazards (disasters) and shocks. Policy makers can use the scorecard as a systematic screening tool to identify focus areas for investment in building more resilient health systems and strengthening their disaster risk management (CDRM) capabilities. The scorecard consists of 80+ individual (mix of quantitative and qualitative) indicators across four pillars of facilities, systems, response, and infrastructure. The indicators cover multiple categories from codes and regulations, physical assets, information systems, to public communications, to name a few. Final scores are stoplight based (“red,” “yellow, “green”), making it easier to spot strengths and existing gaps. Depending on the size and complexity of the country’s health system, along with data availability, it can take anywhere from one week to a month to conduct the assessment. Results can help to identify existing gaps, target specific in-depth analyses, and inform investment operations, including instruments like the World Bank's Catastrophe Deferred Drawdown Options (CAT DDOs), as well as contribute to Country Climate and Development Reports (CCDRs).
2. Deep-Dive Assessment
The deep dive assessment builds on the scorecard’s rapid assessment and uses semi-structured expert interviews and additional research to form a better understanding of health system capabilities implementation on the ground. Relying on data collection from site visits and expert interviews, this deep dive is more resource intensive and is well suited for countries with smaller health systems. In larger countries, it can be tailored for use in subnational regions or focused on specific issues with a narrower scope to achieve pragmatic outputs, informing scalable interventions. The results can be used to support other workflows e.g., cost and benefit analysis of interventions and derive concrete actions for strengthening the resilience of health systems to shocks.
1.Health Facility Master List
The global thematic area can support the Ministry of Health (MoH) and country teams in creating up to date, geo-tagged, health facility master lists with various levels of details for additional facility characteristics, based on country needs and data availability. Advanced data analytics and AI are used to complete missing information and triangulate data accuracy using multiple sources as inputs (OSM, government data, public data bases etc.). Additional facility characteristics most commonly include type of facility, level of care, number of beds, doctors, and nurses, but can be adjusted to specific country needs.
2. Disaster Risk Exposure and Vulnerability
By combining population density, health facility location, and socio-economic vulnerability data with hazard data, granular estimates for exposure and vulnerabilities can be created for various natural hazards, such as earthquakes, flooding, landslides, mass displacements, extreme temperatures (both hot and cold), precipitation, and wildfires. Detailed vulnerability maps can help policy makers and operational teams to identify where people or the health system is most likely to experience disaster impacts and surge demands after a natural disaster. This information is vital in building more resilient health systems and informing health system planning.
3. Vulnerable Population Identification
By adding socio-economic and population health data to the exposure data, country specific, localized population vulnerabilities and the most vulnerable populations can be identified. This information can help MoHs and other ministries in preparing adequately before disasters hit and to protect the most vulnerable populations, that are typically the least able to deal with the impacts of natural disasters.
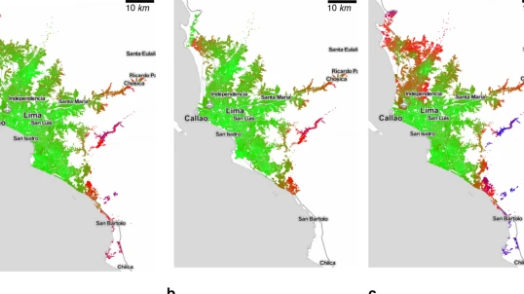
4. Accessibility Analysis
This analysis models accessibility to health facilities by overlapping health facility locations, population density, travel speed, and risk exposure. In a first step, the model estimates hazard exposures of the population, and health and transport infrastructures. In a second step, average travel times are estimated for a “business as usual” scenario and for disrupted scenarios where natural disasters impact roadways and health facilities.The outputs help identify underserved areas where access changes during disasters and people need the longest time to reach any health services. This tool does not only estimate travel time to the closest facility, but also the average travel time to any facility, offering more realistic estimates of health services access, as people in urban areas often do not choose the closest health facility.
5. Infrastructure Criticality Analysis
This tool is used to assess the roles the transport network and other lifelines infrastructure networks play for access and functionality of health facilities and the health facility network. In case of the transport network, the results identify which roads are the most critical in ensuring continued access during routine demand as well as in case of disasters. The underlying methodology and its results are further discussed in this technical paper and emerged from the World Bank Group report Frontline, that presents a framework to increase the resilience of health systems to shocks.
6. E-health Accessibility
This analysis provides a measure for the feasibility of e-health services, by combining population, network connectivity and survey data for internet and communication devices. It can identify areas where e-health services can be a feasible option to supplement physical access to health facilities in times of need. The results can also help to identify areas where e-health services are not feasible. Combined with the accessibility analysis for physical access, this offers a more holistic picture of the population’s ability to access essential health services in a timely fashion.
7. Health Facility Prioritization
This tool identifies the health facilities serving the most vulnerable populations in terms of service availability, e.g., existing feasible redundancies in the health facility network in any region, socio-economic vulnerability and exposure to various hazards. It also considers the vulnerability of facilities themselves and helps identify the health facilities most in need of detailed assessments and upgrading based on their building state, the population they serve and the hazard exposure. Depending on data availability, the analysis can incorporate information on service availability from a supply side, e.g. access to healthcare personnel. An example of this is presented in this paper.
8. Disaster Target Analysis via Gap Clustering (CD-Tag)
The integrated risk index that considers a set of sociodemographic variables with the accessibility and criticality to group administrative units (departments, provinces, etc.) in very high, high, medium, and low risk based on their exposure and vulnerability profile. The first step involves establishing a hazard risk profile, determining socio-demographic variables to be used as proxies for population vulnerability, and collecting and validating geo-located data on a (health, education, energy etc.) system infrastructure. The second step quantifies the population and assets exposed to hazards at the local municipality level by employing spatial intersection techniques. In the third step, all information is consolidated, and each local municipality is defined by multiple characteristics including percentage of facilities exposed to a hazard, percentage of population exposed to a hazard, and a set of socioeconomic factors. The last step uses cosine similarity to calculate the distance between the current state of the local municipality and its ideal state represented by the established targets to determine the exposure and vulnerability level of each region, taking into account complex system interdependencies.
9. Health Facility Surveys and Intervention Guides
This involves designing (rapid and deep dive) health facilities (primary, secondary and tertiary) surveys for target countries. The goal of the surveys is to assess the healthcare systems operational functionality and resilience outlook. Consisting of 500+ questions, the deep dive survey helps assess healthcare facilities against multiple hazards e.g., floods, storms, landslides, seismic activity, heatwaves, and wildfires, etc. The surveys/questionnaires are divided into multiple sections including hazard exposure, health workforce, water, sanitation and healthcare waste, energy, and infrastructure, technologies, products and processes which assists paint a broader picture of services, resources, and operational capabilities. The outputs then help government agencies and local authorities design intervention guides as well as facilitate a cost assessment for facility rehabilitation and renovation.
10. FCV Health Resilience Outlook via Satellite Imagery
Health services are severely impacted in fragility, conflict and violence (FCV) contexts. This analysis uses satellite imagery (Sentinel-1 among others) and AI modeling to assess the extent of damage to healthcare facilities in high conflict areas across a country. In a time-series analysis, combining radar and optical imagery from sensors, this satellite-based framework measures both the degree of damage and recovery of hospitals following conflict. Damage is identified by comparing satellite observations from before and after conflict periods, using statistically robust change detection methods over time series data. This allows the project to distinguish meaningful, conflict-related structural change from normal background variability. The result is a spatially explicit measure of damage intensity, rather than a simple damaged/not-damaged classification. These physical changes are reflected in satellite observations over time and can be translated into interpretable indicators of damage severity and recovery progress.
1.Green, Resilient, and Inclusive Health Facilities – Guidelines
This guidance note collates global knowledge products and existing guidelines to help operational teams to assess the state of the art and global best practices for building green resilient and inclusive health facilities. The guidance note is developed in close collaboration with GFDRR’s thematic line for building regulations for resilience.
2. Roadmap for Resilient Health Systems
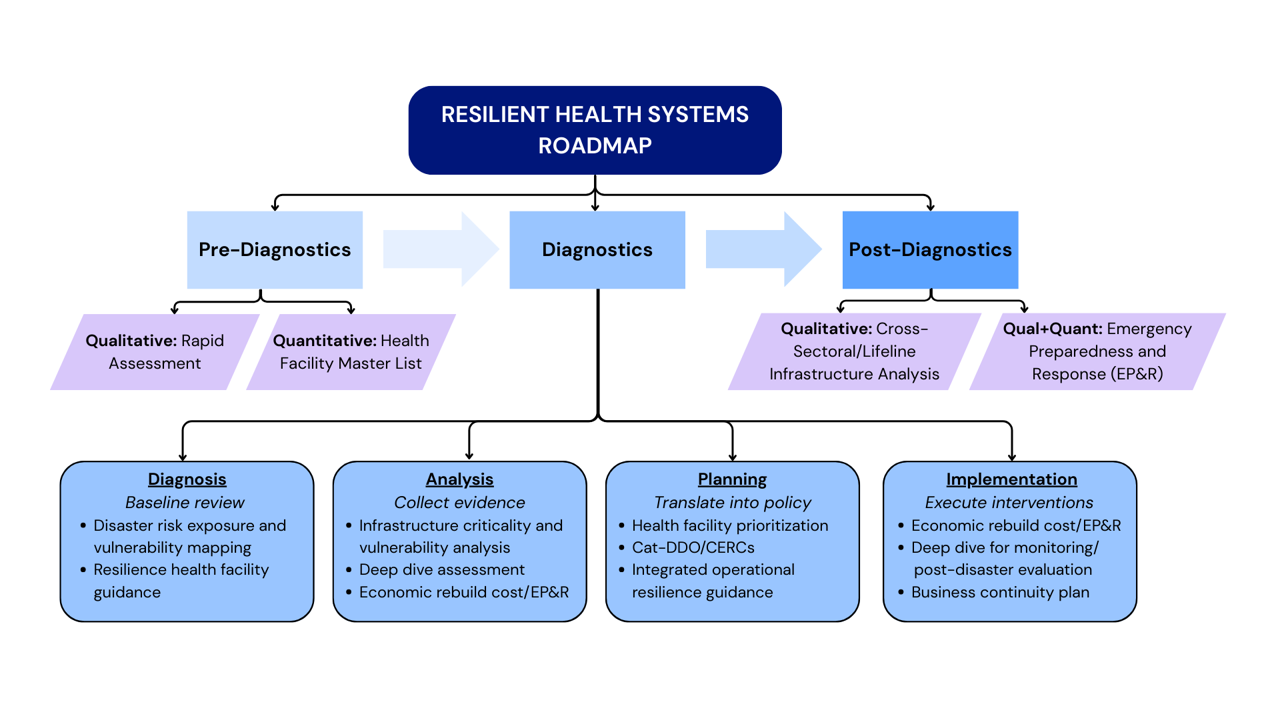
The Roadmap for Resilient Health Systems (RRHS) is a step-by-step guide to help governments strengthen health systems to withstand and respond to crises. Consisting of three main phases [pre-diagnostics, diagnostics (diagnosis, analysis, planning, implementation), and post-diagnostics], it provides tools to identify vulnerabilities, prioritize measures, and invest in resilient services. By linking health systems with lifeline infrastructure, the roadmap supports policymakers in moving from reactive crisis management to proactive resilience building—ensuring essential care continues during emergencies and protecting long-term development gains.
3. Safer Clinics Framework
Inspired by the World Bank Group’s Roadmap for Safer and Resilient Schools (RSRS), the 5S Framework (space, stuff, staff, system, social) is aimed at helping build safer clinics. It focuses on five major areas crucial to evaluate the safety and functionality for clinics and healthcare facilities, especially during hazards. It helps countries determine the condition, capacity, and preparedness of existing clinics’ infrastructure, availability of basic as well as emergency medical equipment and resources, the extent of safety of all staff necessary to provide services, proficiency of healthcare operations, policies, system management plans, and financial mechanisms and lastly, availability of community services and integrations of larger social plans. The framework has three main steps: diagnosis, analysis, and planning to help (1) collect information and establish a quantitative/qualitative database, (2) analyze the information to assess capacities, needs, and potential risks/challenges in planning and (3) design an intervention strategy is designed to implement solutions.
4. Preparing Health Systems for Shocks : Japan’s Experience of Enhancing Resilience of Health Systems
This report focuses on Japan’s experiences to showcase how the country incrementally strengthened the resilience of its health system by enhancing its capacity to prepare for, respond to, and recover from crises, drawing valuable lessons from its experience of major earthquakes, floods, and infectious disease outbreaks. It outlines how, the health sector, disaster risk management, and quality infrastructure, were integrated through the development of key regulations, governance mechanisms, and capacity building for all stakeholders involved in strengthening the health system's ability to withstand shocks. By providing practical reference material the report highlights best practice examples and case studies to inform and inspire shock-resilient policy reforms and infrastructure investments
Resilient Health Systems Roadmap
The Roadmap for Resilient Health Systems (RRHS) is a step-by-step guide to help governments strengthen health systems to withstand and respond to crises. Consisting of three main phases [pre-diagnostics, diagnostics (diagnosis, analysis, planning, implementation), and post-diagnostics], it provides tools to identify vulnerabilities, prioritize measures, and invest in resilient services. By linking health systems with lifeline infrastructure, the roadmap supports policymakers in moving from reactive crisis management to proactive resilience building—ensuring essential care continues during emergencies and protecting long-term development gains. We are in the process of finalizing the detailed roadmap but below is a quick snapshot.
Knowledge Products
Our Global Footprint
Our work spans 30 countries across five regions, supporting governments in strengthening health resilience to a wide range of disaster risks, including floods, heatwaves, and landslides. We operate at the intersection of health and other critical sectors—including energy, education, transport, and Fragility, Conflict and Violence (FCV) and have supported a diverse portfolio of World Bank operations.